| Figure 1. Atrophy of the Brain in MS |
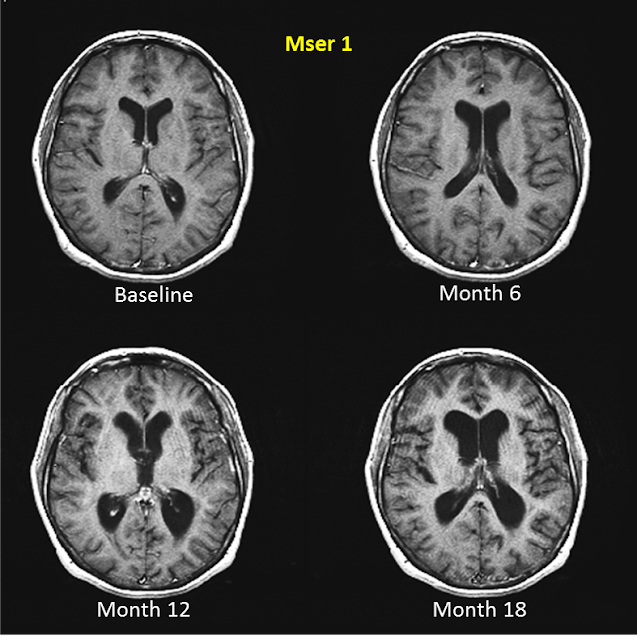 |
| An individual with MS was followed for a period of 18 months. During this time, significant atrophy in the brain was observed. http://multiple-sclerosis-research.blogspot.ca/2013/06/rebranding-ms-as-dementia.html |
"I've had MS since 1975. I don't know how many relapses I've had. I don't know what all my symptoms are. That is the problem. MS wears many masks." - Anonymous MS Patient Source: http://ms.about.com/u/ua/livingwellwithms/user_coping.htm
Multiple sclerosis (MS) is a debilitating disease that imposes vast limitations on an individual’s ability to function in their everyday life, primarily as a consequence of the associated effects of demyelination of the central nervous system. To explain the pathogenesis of MS, neuroscientists have traditionally focused their efforts on understanding white matter pathology. White matter pathology has been found to be characterized by such features as focal demyelinated plaques that are often associated with a host of inflammatory pathways [1]. However, recent advancements in the field of neuropathology have allowed for the closer examination of grey matter tissues and its correlation with the disease symptoms of MS. Closer examination of the grey matter pathology of MS has revealed characteristic features that allow them to be distinguishable from that of white matter [1]. These differences suggest that the disease phenotype presented in MS must be a result of the combinatorial effects of both types of neural tissue changes. Moving forward, it is only by gaining a deeper understanding of the changes in both the white and grey matter of the brain that we are able to sufficiently explain the deficits shown in individuals with MS.
|
Table of Contents
|
3.1 The Overall Pathogenesis of MS
The propagation of MS, an autoimmune disease wreaking havoc on the central nervous system, is plagued by a number of unknowns. It remains to be determined what steps allow for the initiation of multiple sclerosis, as well as how the disease evolves over time. Two hypotheses explaining these steps are currently at the forefront of neuroscience; MS as an immune initiated disease, and MS as a neural initiated disease.
| A Closer Look At the Pathogenesis of MS |
| This animation provides a simplified description of the pathogenesis of MS. |
3.1.1 MS as an Immune Initiated Disease
The proposal of MS as an immune initiated disease, suggests that injury inflicted on neural tissues is induced by an inflammatory cascade instigated by the T cells of the immune system [2]. This hypothesis draws from the findings presented in a number of studies that identify cells of the immune system as being the culprit in initiating multiple sclerosis. Bielekova et al. (2004) detected a higher frequency of CD4-positive myelin reactive cells in the peripheral blood of individuals diagnosed with MS, in contrast to the levels detected in healthy individuals [3]. This result is indicative that there is prior sensitization of T cells to antigens related to MS in those individuals suffering from the disease [3]. In addition to the activities of CD4-positive T cells, contributions made by antibodies, another cell of the immune system responsible for targeting the myelin ensheathing axonal projections, is an important determinant of the degree of neural injury inflicted [4].
3.1.2 MS as a Neural Initiated Disease
The proposal of MS as a neural initiated disease suggests that, following the persistent infection of a small grouping of neural cells, the consequential release of tissue antigens is sufficient to incite an autoimmune response, which ultimately evolves into MS [2]. This model of pathogenesis is based on the pathway followed by Theiler murine encephalomyelitis virus, which provokes a disease with marked similarities to MS [2]. In the development of MS, the Epstein Barr virus is thought to act as the causal agent [2].
3.1.3 Propagation of MS
Despite uncertainty surrounding how MS becomes initiated within an individual, studies have revealed the overall discourse of the disease. Damage inflicted on oligodendrocytes and neurons, by the actions of immune cells, leads to the severe debilitation of nerve conductance in the central nervous system [5]. This is because, within the central nervous system, there is recognition of fragments of myelin, which have been displaced by immune cells. This recognition acts as the catalysis to neural tissue damage and the formation of lesions. In response to such damage, inflammation occurs, and results in further degradation of myelin, as well as the loss of axons and neurodegeneration. The underlying mechanisms implemented by the immune systems vary, and result in four subtypes of MS, which differ in terms of the temporal progression and severity of symptoms [5].
3.2 Features of MS Pathology
There are a number of pathological hallmarks associated with MS. The onset of MS is marked by the appearance of pathologic lesions, which form as a consequence of inflammation, demyelination and remyelination, neurodegeneration, and astrogliosis [12]. These lesions possess characteristic inflammatory features due to the degradation of myelin and phagocytic activities taking place within neural tissues [2]. These lesions are found in a number of areas throughout the brain, including the optic nerves, the subpial spinal cord, the brainstem, and the cerebellum [12]. The evolution of such pathologic lesions varies throughout the course of MS, as the type of lesions that will develop is dependent upon the stage of MS, how quickly the lesions can progress, and the degree of remyelination.
| Figure 2. Histological Characteristics of MS Lesions |
 |
| Active phagocytosis of myelin fragments during the early phases of lesion formation is associated with the presence of macrophages. http://link.springer.com.myaccess.library.utoronto.ca/article/10.1007%2Fs00401-012-0953-0 |
3.2.1 Features in White Matter
The lesions present in white matter, which include active lesions, inactive lesions, smoldering lesions, and shadow lesions, have been found to be distinguishable from one another.
- An active lesion is a demyelinated lesion characterized by the preservation of axons, and the infiltration of macrophages [5]. Active lesions can be categorized as either acute or chronic depending upon their longevity.
- An inactive lesion can be characterized by a loss of axons and oligodendrocytes, as well as the absence of macrophages [5].
- The intermediary form of lesion, termed the smoldering lesion, is characterized by a hypocellular center, and the aggregation of macrophages around the periphery [5].
- There are also shadow lesions, which have undergone a degree of remyelination [5]. However, these shadow lesions only appear during the early stages of MS, and may represent a phase in which remyelination is possible.
The incidence of white matter lesions varies across the different subtypes of MS. It has been found that in both relapsing remitting MS and secondary progressive MS, active lesions develop [5]. In contrast, in primary progressive MS and progressive relapsing MS, inactive lesions develop [5].
3.2.2 Features in Grey Matter in MS
| Figure 3. Grey Matter Lesions |
 |
| The lesions of grey matter are shown in panels A-D. http://openi.nlm.nih.gov/detailedresult.php?img=3262750_1471-2377-11-153-2&req=4 |
Although MS has traditionally been perceived as a disease plaguing the white matter tissues, the identification of grey matter pathology improved neuroscientists’ ability to explain all of the deficits presented in MS. The appearance of lesions in grey matter occurs in both the early and late stages of MS [5]. These lesions are categorized into type I lesions, type II lesions, and type III lesions.
1.Type I lesions have been defined as having a leucocortical location and are not confined to the grey matter, but also have the capacity to spread to adjacent white matter tissue [6].
2.Type II lesions have been defined as having an intracortical location and are confined to the cortex [6].
3.Type III lesions have been defined as being located parallel to the pial surface [6].
The development of research focused on grey matter pathology has allowed for neuroscientists to better understand the consequences associated with atrophy in this tissue. Specifically, it has revealed the undeniable association between declines in cognition and the progression of lesions in grey matter [1]. This was exemplified in a study performed by Morgen et al. (2006) in which performance on the PASAT, a neuropsychological test, was found to be strongly correlated with the volume of grey matter in patients with MS [7].
3.2.3 The Relationship Between White Matter and Grey Matter Pathology in MS
The complexity of multiple sclerosis and its ability to alter the landscape of the brain’s tissue have made it difficult for neuroscientists to delve deeper into understanding of how the disease’s components influence one another. To determine the type of relationship linking together lesions of white matter tissues and the atrophy of grey matter tissues in MS, Muhlau et al. (2013) employed magnetic resonance imaging (MRI) techniques [8]. MRI was used to garner cross-sectional images of the brains of two hundred and forty-nine patients with relapsing-remitting MS. Results indicated that there were spatial associations between the atrophy occurring in grey matter, and the lesions appearing in white matter [8]. These spatial associations are important in demonstrating that grey matter atrophy is influenced by the axonal pathology of white matter lesions.
3.2.4 Features of Normal-Appearing White Matter
The injury inflicted in the brains of those with MS is not solely localized to the sites of lesions, but instead can be widespread throughout the entire brain. For example, a number of processes, including inflammation, the activation of microglia, astrocytic gliosis, demyelination, and the loss of axons, occur in normal-appearing white matter [9]. To assess the axonal loss in the normal-appearing white matter of deceased patients with MS, measurements of both axonal density and the atrophy of white matter were taken [10]. Findings indicated that there was a significant reduction in both the number of axons present, and the density of axons in comparison to healthy controls [10]. Such findings exemplify the types of changes that occur in normal appearing white matter, but are inconclusive in terms of defining what type of affects these changes have. In order to determine how changes in normal appearing white matter translate to the development of the deficits seen in multiple sclerosis, Filippi et al. (1995) had twenty-seven individuals with multiple sclerosis undergone magnetization transfer imaging (MTI) [11]. The results from this imaging technique were then compared to healthy controls. It was found that in those patients with multiple sclerosis, the mean magnetization transfer ratio was lower in frontal white matter regions [11]. Additionally, it was also found that normal-appearing white matter located adjacently to lesions had magnetization transfer ratios that increased with distance away from such sites [11]. The patterning identified in this study is important in helping to reveal the types of changes that appear in normal-appearing white matter, and how such changes influence the appearance of disability in multiple sclerosis.
3.3. Areas of Further Research
It is imperative that research focused on the neuropathology of MS continues to expand. This is because improvements must be made in both our understanding of how MS progresses, and our ability to apply new diagnostic and treatment strategies. Due to the novelty of research centered on grey matter pathology and MS, current treatment strategies do not consider the role of grey matter in influencing the severity of the disease. One area that will surely be a strong candidate for further research involves epigenetics as this field is closely linked to the pathology of MS [5]. Furthermore, in order to gain a better understanding of the driving forces behind MS, the employment of techniques, such as two photon microscopy, and the imaging of cellular components will be important in the future [5]. Only through the implementation of innovative techniques will neuroscientists have the ability to unlock the secrets of this potent disease.
Overall, great work! I like how you started off with a quote of someone living with MS. It provides an important and different perspective on the disease. The video and images also help visualize the underlying pathology.
My mother is a sufferer of M.S and I'd always been to scared to do any research on it. This really helped me to understand some of the pathology of the disease. This page is organized really clearly and it was easy for me to understand, especially because I have no other knowledge about M.S. Thanks!
I agree with Cassandra Anor, I really like how you started the content by sharing a quote from a patient suffering from multiple sclerosis. I am really you are one of the few people that have thought about this. Really like thinking outside the box. And an excellent video on explaining the neuropathology of multiple sclerosis.
The quote was a great idea that added a personal touch on the topic. The differentiation between the effects on grey matter and white matter in conjunction with the figures that the show lesions respectively helped with the understanding immensely.
I like how you organized your topic, and the detail about the features of white matter and grey matter! You conveyed a lot of information and the images complemented your descriptions nicely! Great job!